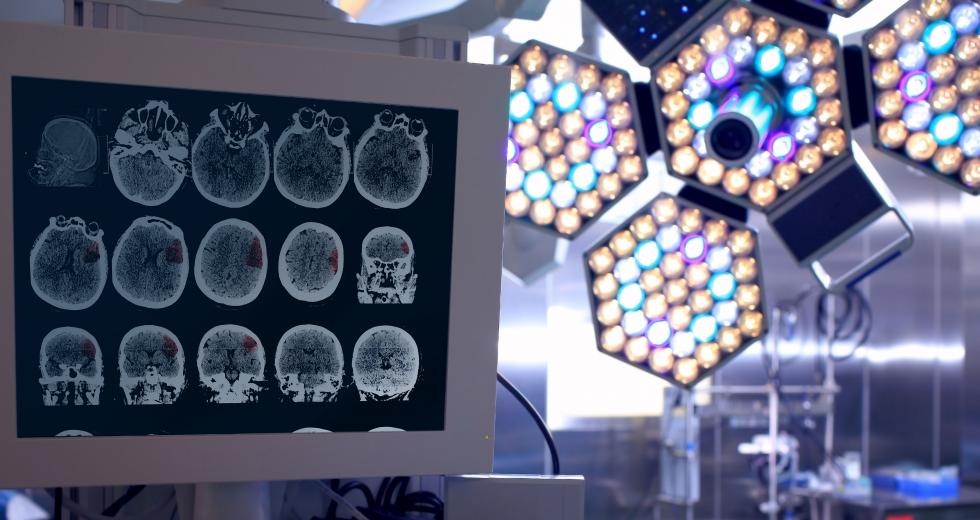
As a radiation oncologist with Sutter Health, Dr. Harvey Wolkov spends his days zapping tumors and other types of lesions from patients’ brains with gamma rays. It’s a tricky job because, during the procedure, patients aren’t allowed to move, even a fraction.
To hold patients perfectly still, a neurosurgeon would typically attach a box-shaped metal frame to the head, fastened by four screws in the skull. The device was clunky and uncomfortable, but this immobilization system helped with accuracy. Plus, it was the only viable option at the time, Wolkov says.
Times have changed. The Sutter Neuroscience Institute in Sacramento now has a new machine: a $7 million, 21-ton gamma knife that allows patients to undergo radiation therapy without a headframe. Instead, they wear a frameless mask, which is more like a hot towel on the face during a spa treatment.
In March, the institute’s Sutter Gamma Knife Radiosurgery Center became the first site in the U.S. to use this new system — designed to make brain surgery faster, safer, quieter and more efficient than older models.
The first patient, Steven Ramsey, 52, of El Dorado Hills, had a metastatic brain tumor. Sutter’s gamma knife team molded the frameless mask on his face, then began the procedure, running controls from outside the high-density concrete vault.
With previous technology, these operations can take hours because of the prep time needed to do imaging and set up the headframe. But Sutter officials say the new machine can cut the treatment time down to 30 minutes. Additionally, this system provides as much accuracy as the old one, but the mask allows the brain surgeons to administer multiple fractions of radiation over several days. This method can protect healthy brain tissue from damage, as opposed to giving patients one large dose of radiation, which is more likely to damage surrounding tissue.
“The technology will serve patients very well,” Wolkov says. “It will allow us to deliver multiple treatments over three or five days, which has the potential to decrease side effects when treatment is delivered near sensitive critical structures, such as the optic nerves.”
The new machine — called the Leksell Gamma Knife Icon — comes from Sweden-based Elekta, a leading supplier of advanced radiation oncology and neurosurgery systems. The Icon is the sixth generation of the system, based on advances developed throughout the company’s 30-year history in stereotactic radiosurgery technology. Medical centers in Europe and Asia have already started using this device. Several U.S. sites have purchased the system, but await installation. But there are always obstacles with bringing new technology to the medical arena, such as a learning curve, familiarity with the old system and regulatory hurdles.
“Fortunately, Sutter staff, working with Elekta, expertly handled these challenges and cooperated well with the state of California and national authorities,” says Bill Yaeger, Elekta’s executive vice president in charge of North America. As of March, the Sutter Gamma Knife Radiosurgery Center had treated eight patients with the new machine.
But the learning curve is real. These first treatments took longer than they would have with the previous system, Wolkov says. He expects that to change as the team adjusts and starts making the mask a day before treatment. The frameless mask may be more comfortable, but immobilization still matters: “If they’re even twitching their nose, that will cause us to move slightly out of spec and the treatment will be interrupted.”
The patient motion management system can be finicky — any movement of the head greater than 1.5 millimeters for more than two seconds, and the machine shuts off, which means a portion of the procedure may have to be repeated. Most patients have no trouble lying still. One patient, however, fell asleep during surgery and his snoring interrupted treatment. Wolkov says the team had to wake him up and tell him not to move.
For more on local medical advancements, stay tuned for Russell Nichols coverage of stroke technology, including this month’s cover story, “Hour of Need.” Sign up for our newsletter, and we’ll email you when it’s available online.