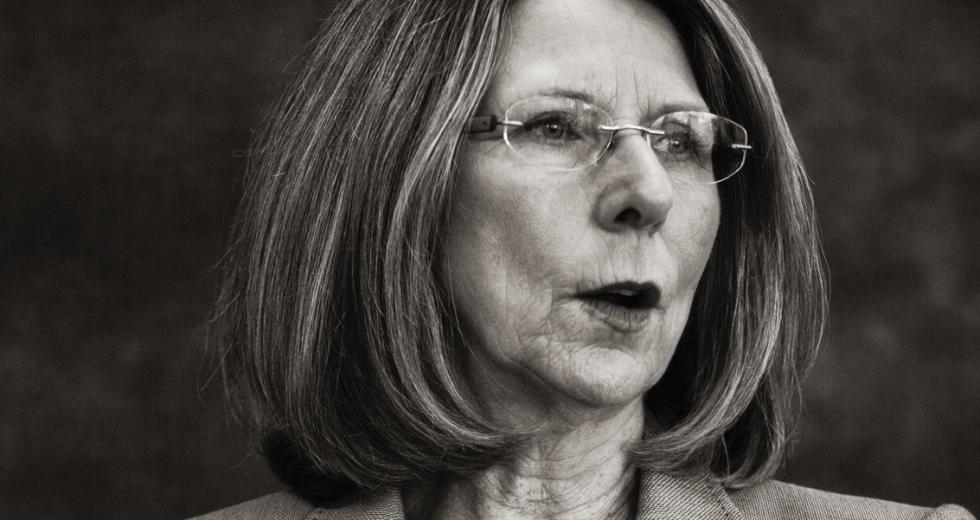
You would be hard pressed to find anyone with a greater breadth of understanding and experience in navigating the complex Golden State health care system than Diana Dooley, California’s secretary of Health and Human Services. Born and raised in the Central Valley, Dooley has spent the bulk of her professional life working in health advocacy, most of it on behalf of California children. These days, she is also the chair of the California Health Benefit Exchange Board, the agency tasked with implementing the online insurance marketplace, dubbed Covered California, that is critical to the success of the Affordable Care Act. We sat down with her recently to talk about the agency’s progress and challenges in implementing this historic change in the American health system.
Comstock’s: First, will California be ready to begin
enrolling people in health benefits exchanges on Oct. 1 and to
fully implement the Affordable Care Act (Obamacare) by the Jan.
1, 2014 deadline?
Dooley: Those are two very different questions. We are
going to be ready. It will be in the fall, but it may be a little
past Oct. 1. Even so, we have planned for three months of open
enrollment prior to January, so if it isn’t Oct. 1 we still
haven’t lost a lot. And then the open enrollment is going to go
for 30 days into the new year, so we’ll have a cushion. But we
are on track with all of the markers that we have set, and we
will offer coverage on Jan. 1. The biggest challenge, as always,
is building the IT system. We are on a very compressed schedule,
so even with a very reliable vendor, with the very best people
and all the resources and with the federal government putting up
all the money to get this built on time, things can still go
wrong.
Comstock’s: There are some big names among the health
insurers who have opted to not participate in the exchange. Are
you satisfied with the options consumers will have?
Dooley: I’m very satisfied. We made it very clear that
we wanted to have a partnership relationship with the plans and
the providers, and we have all of the major players in the
individual market. There’s been some press about Aetna and United
(Healthcare Services Inc.) not participating, but those two
companies have less than 7 percent of the individual market.
Since then, Aetna has also announced they’re getting out of the
individual market in California in favor of the employer market,
which is their own business model. We invited all comers, there
was no one excluded. We had over 33 issuers that expressed an
interest, and they all looked at what the conditions are going to
be and what their own business needs were. They’ve agreed to all
of our terms and conditions and are in it for the long haul, as
are we. So I’m very satisfied that the plans in the exchange are
qualified health plans.
Comstock’s: Medi-Cal, the state/federal health
insurance plan for the poor, is a huge concern here, too.
California has accepted the ACA’s call to expand the program, and
the federal government will provide 100-percent reimbursement for
new Medi-Cal (Medicaid) patients for the first three years. That
eventually drops to 90 percent in 2020, but some believe that
level could be volatile. Here in California, we passed
legislation allowing us to opt out of Medi-Cal expansion if
federal cost-sharing drops below 70 percent. Did our lawmakers do
enough to protect California financially?
Dooley: I think in the process of the budget overall,
there was a very good give and take, and I’m very comfortable
with where they settled. Fiscal uncertainty has always been a
concern with things that involve federal participation. But we
have a backstop if a funding cut happens. As you said, the
federal rate won’t reduce to 90 percent until 2020. I think part
of that was in recognition that these people who will be newly
eligible have been left out of the system for some time. They
have not had regular care, so there will likely be some
additional cost at the beginning that should level out over time.
When we do shift in 2020, I hope we’ve been as successful at
moving people into systems of care that promote health and are
costing the health care delivery system less.
Comstock’s: What are some of those cost-control
elements?
Dooley: There are many. For one, we’re changing how we
manage people who are eligible for both Medicare and
Medi-Cal. Not all Medicare recipients are seniors; there are
people on Medicare with disabilities, and if they’re totally
disabled they’re on Medicare at a younger age. Many are so low
income that they’re also eligible for Medi-Cal. So there are
different services that are paid for by either program, and they
have been completely uncoordinated in the past. The Affordable
Care Act provides a way for us to better coordinate that care and
to offer incentives to provide care in a more efficient way. One
of the principles of the Affordable Care Act is to move away from
a fee-for-service model to a payment-for-outcomes. So right now,
you get paid for how many procedures, how many tests, how many
office visits. California has been a leader in managed care where
we pay a capitated rate. Kaiser is the best example, but there
are many other health management organizations that take an
amount of payment per enrolled person and then they manage that
care in a way that lowers cost. So we’re pushing to expand that
even further.
Comstock’s: There has been strong concern among
hospitals that the ACA penalizes them with lower payments when a
patient has to return to the facility within a short time for the
same problem. Can you explain this?
Dooley: This is primarily in the Medicare program. The
state doesn’t have much to do with the management of the
situation, though we are looking at how it impacts the
duel-eligibility people I mentioned. I think all health care
observers believe that when you are discharged from the hospital,
there should be a plan for your effective care. If you have to
come back into the hospital within 30 days, there’s a presumption
that you didn’t get the right discharge care, you didn’t get the
right planning, you didn’t get the right follow up. So the
readmission rates under the Affordable Care Act are designed to
give hospitals the incentive to put the right discharge planning
team together. It could be as simple as having a case manager at
the hospital following up with the primary care doctor to be sure
a patient has come in for his appointment or who will call the
patient to be sure they are taking their medication.
Comstock’s: That would seem to be a real benefit for
older patients. So much of our health care comes in the latter
stages of our lives, and nobody wants to be in the hospital if
they can avoid it.
Dooley: And everybody needs help. We all need a health
advocate. We all need somebody to help us understand the
medications or check to see if we’re taking them. A lot of people
don’t have a partner there to help them late in life. I think
there are a lot of advantages, but it does require an
understanding that we’re looking to improve quality. We will also
save costs, but it’s a mutual need.
Comstock’s: So much of the success of the ACA in
California is going to depend on getting as many eligible people
as possible into the system. I know you’ve been working hard on
an outreach plan to educate Californians about all this. How will
that outreach plan work?
Dooley: Our outreach in education is in three basic
categories of activity. The first is a series of training grants
issued to about 48 community organizations who are being trained
on the operation of the product and how to be enrolled and what
the ACA is about. That started in July. The second part will be
actual enrollment. We’ll have perhaps as many as 20,000
enrollment counselors throughout California. Some will be
employees and volunteers within these community organizations,
and some will be employees of providers, hospitals, clinics and
doctors’ offices. Those enrollment counselors will all be
trained, they will have background checks and they will be
certified as competent and responsible to help people actually
enroll in Medi-Cal or Medicare. The third part will be the
broadcast messages — radio and television and billboards and
flyers. The federal government will also be running its own
campaign that will go on across the country for how to enroll and
what the Affordable Care Act is. So it’s a tiered process going
from the top with the national messages to our broadcast messages
in California to the outreach of the community groups that are
trusted by the people of our state.
Comstock’s: We often talk of “known unknowns” vs.
“unknown unknowns.” With so much of this still in the latter
category, what is your biggest concern at this point?
Dooley: I see full implementation and a fair assessment
of success being about two or three years out. I think a lot of
people will want to define success much sooner than that, but
this is going to be a big lift for a long time. We have in our
projections at Covered California a baseline and an enhanced
objective to meet for enrollment. Clearly, the ultimate success
is people getting the care they need, and that’s at the very end.
What we have to do right at the beginning is get people the
coverage they need. I think we have a very good plan, but there
are still a lot of places where we can go off track. We’re on
track now, but we’re going to have to stay with this and be
nimble and be willing to make course corrections, as we have
getting to this point. If so, I think we have a fair chance at
making a lot of lives better in California.
Comstock’s: Does the Obama administration’s decision
to delay mandating large employers to provide workers with health
care impact anything we are doing here in California?
Dooley: We don’t believe it does. It definitely doesn’t
have any impact on small employers. We will continue to seek
further guidance from the administration regarding individuals
who say they are employed by a company that doesn’t offer
insurance or for one where the insurance is unaffordable, but it
should not in any other way affect us.
Comstock’s: What does your gut tell you about what
this means for the overall health of the law?
Dooley: We have a very complicated system, far more so
than when we created Medicare and Medicaid 50-plus years ago.
It’s also far more complicated to change an existing system than
it is to create one from whole cloth the way we did with those
programs. Given that complexity and that we’re modifying it in
very significant ways, there are going to be places where it
won’t work exactly as it was originally designed. That’s why the
U.S. Secretary of Health and Human Services (Kathleen Sebelius)
has the flexibility to reconcile these issues and to make the law
work. At the state level, we also know there are going to be
times when we need to make course corrections, whether
administratively or within the law itself. We won’t know until we
get a little further down the road. These are big programs with a
lot of moving parts, but we will be able to make our rules on the
basis of actual practices. We’re still speculating about a lot of
what could happen, so the more data we can gather as we go, the
better we can accommodate the Affordable Care Act’s goals.
Recommended For You

Paging Dr. Bera
Seeking remedies in the halls of Congress
U.S. Rep. Ami Bera has spent most of his career as one of the Capital Region’s leading voices on health care, first as a doctor and later as Sacramento County’s chief medical officer and a dean of admissions for the UC Davis medical school.

Are Attorneys the Rx For Obamacare?
Changes in healthcare shift law agencies into high gear
Hospitals, law firms and state agencies involved in implementing the Affordable Care Act have seen a sizable bump in workload — and in some cases, staff sizes — as they prepare for the major overhaul mandated by the 2010 law and to adjust to other industry changes.