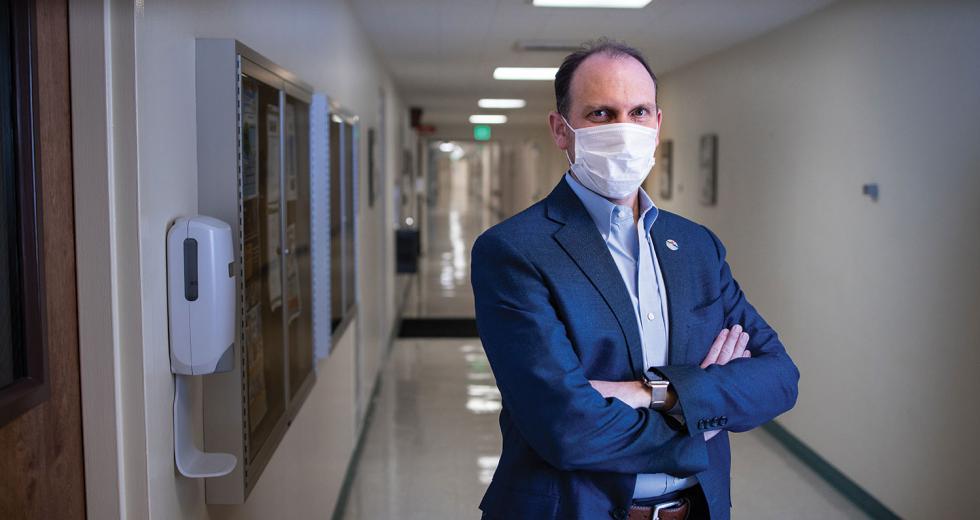
Daniel Wolcott, president and CEO of Dameron Hospital in Stockton, was walking a corridor on the COVID-19 floor in early July when he encountered a fully outfitted nurse: gown, N95 mask, face shield. He asked how many times she changed her gear during each 12-hour shift. It was every hour or two — eight or nine new sets of personal protective equipment each shift. It reminded him of the courage of those holding the line on the coronavirus crisis. “Out of a 12 hour-shift, a nurse is staying in this very hot and sweaty PPE equipment for probably eight to nine hours out of the 12,” Wolcott, also president of Adventist Health Lodi Memorial, says.
It illustrates something else too: what the pandemic has done to hospital finances. New requirements and soaring prices ballooned PPE costs per patient per day from an average of 35 cents pre-pandemic to almost $26 in April, according to the Society for Healthcare Organization Procurement Professionals — a more than 7,300-percent increase. That’s not all: The pandemic has forced hospitals to invest in clinical equipment, technology and infrastructure for telehealth visits, ventilators and empty beds to accommodate surges.
The Capital Region’s hospitals are the lifeboats against the repeated swells of this coronavirus. The biggest systems are being hit with huge losses. Sutter Health, which runs eight hospitals in the Capital Region, reported that in April alone it lost $168 million, or 19 percent below break even — even with factoring in $200 million in federal bailout money. Kaiser Permanente, which operates six hospitals in the Capital Region, posted a $1.1 billion loss for the first quarter.
But experts say it’s not those big systems whose survival is at risk. It’s smaller, independent hospitals like 200-bed Dameron. If it and others go under, it would leave holes in health care systems at a time when coronavirus has been surging. Their failure would also drain much-needed jobs and spending out of the region at a time of economic crisis.
Hospital closures outside major metropolitan areas can be bad news for health and the economy. Distance to hospitals matters for survival. An August 2019 National Bureau of Economic Research study of 92 hospital closures in California found that rural hospital closures increased inpatient mortality by almost 9 percent.
Hospital shutdowns also have economic impacts. A 2004 study found that the closure of the sole hospital in a community cuts per-capita income by 4 percent and increases the unemployment rate by 1.6 percent. Dameron is San Joaquin County’s fourth-largest private employer. Marshall Medical Center in Placerville, another independent hospital that also has several outpatient clinics, is El Dorado County’s second-largest employer. Two hospitals in Nevada County — Tahoe Forest Hospital and Sierra Nevada Memorial Hospital — are among the five biggest employers there, public or private.
‘Tweeners’ in Jeopardy
The crisis has shredded hospital budgets. Nationally, April was the worst month ever for hospitals financially. Even before the pandemic, nearly 40 percent of California hospitals had negative margins, according to a May report by health care consulting firm Kaufman Hall. Now they’ve seen possibly permanent reductions in the number of nonurgent but often important elective procedures — almost a quarter of Americans said they’d wait a year or longer to schedule an elective procedure in a hospital, and one in 10 said they would not reschedule at all.
That matters because elective procedures — say, back surgeries and heart procedures — are “where hospitals and surgical practices make all their money,” says Bert Orlov, director of the health care consulting group at EisnerAmper, which has an office in Sacramento. “The revenue loss from COVID-19 for California hospitals is devastating, presenting a financial shock never before felt and likely reshaping the future healthcare landscape,” Kaufman Hall’s report says.
Area health care experts say the bigger hospital systems will survive because they have reserves and willing creditors. The smallest also may do fine — a few rural hospitals like Tahoe Forest are designated as “critical access” and get extra help from the federal government. So those most at risk are what Jeffrey Johnson, Western U.S. market leader for consulting firm Wipfli, dubs “tweeners” — independent facilities that serve smaller towns and cities rather than major metro areas.
Dameron is one of those tweeners. The hospital was losing money pre-COVID — more than $18 million in 2018, the last year for which state data are available. So Dameron came to an agreement last December to be managed by Roseville-based network Adventist Health as an interim step to full acquisition by Adventist. That would be good for Dameron’s long-term viability since hospital networks have more negotiating power.
Revenue for Dameron Hospital, a 200-bed facility in Stockton,
fell by 40 percent in April, possibly putting a deal to be taken
over by Adventist Health in jeopardy.

Now the deal is in jeopardy. Wolcott, who also oversees Dameron during the transition, says the Stockton hospital hasn’t issued any financial statements post-COVID and doesn’t publish its financials. But in April, Dameron’s revenues fell by 40 percent as the hospital stopped elective surgeries, Wolcott says. The hospital was seeing the number of those procedures start to come back in early June when COVID-19 cases started spiking again. That could mean another drop in volumes.
If the case spike goes on another six weeks, “it could potentially inhibit Dameron’s ability to be successful in the long term,” says Wolcott. “If we’re not able to get Dameron turned around to the place where Adventist Health believes it can be successful over time, then Adventist Health can’t afford to just acquire a failing hospital. … Stockton could potentially lose a community asset that provides choice for half a million people.” (State listings show six other hospitals in San Joaquin County: Adventist Health Lodi Memorial, San Joaquin General Hospital, St. Joseph’s Medical Center, Sutter Tracy Community Hospital, Doctors Hospital of Manteca and Kaiser’s Manteca Medical Center.)
“If we’re not able to get Dameron turned around to the place where Adventist Health believes it can be successful over time, then Adventist Health can’t afford to just acquire a failing hospital. … Stockton could potentially lose a community asset that provides choice for half a million people.”
DANIEL WOLCOTT PRESIDENT, ADVENTIST HEALTH LODI MEMORIAL PRESIDENT AND CEO, DAMERON HOSPITAL
At 125-bed independent Marshall Medical Center in Placerville, it’s also been a tough few months. Revenue dropped 30 percent in March, says CEO Siri Nelson. April was worse, but May was not as bad as April. On April 7, credit rating agency Fitch Ratings downgraded Marshall’s bond rating to BB+, technically the highest junk bond rating. Fitch cited a variety of factors: a higher debt-to-cash ratio because of planned building projects, a bigger pension contribution and the impact of the COVID-19 crisis.
Nelson points out that ratings agencies also dinged big hospital systems because of the pandemic. Two of them downgraded Sutter Health’s bonds in April, though they’re still A-rated. Nelson is staying positive. “We’re used to adapting,” she says. Still, she acknowledges that it’s tougher not having a “deep pocket like a big system” nor being cost reimbursed like a smaller critical-access hospital.
Several other small independent hospitals in the region contacted for this story either declined to speak or didn’t respond to requests for comment. One of those, Doctors Hospital of Manteca, is a 73-bed facility in San Joaquin County. It lost $11 million in 2018, the latest year for which data are available. Two others — 111-bed Barton Memorial Hospital in South Lake Tahoe and 152-bed San Joaquin General in French Camp — posted solid income gains for 2016, 2017 and 2018. No state data are available for 50-bed NorthBay VacaValley Hospital in Vacaville.
As bad as the financial impacts have been in the first months of the pandemic, the long term could be worse. “The timeline is even more scary than you might think,” says Orlov. The summer case spike wasn’t the much-feared second wave but the second peak of the first wave. When infection rates dropped in May and June, getting people to come back to the hospital for elective surgeries went slower than hoped, he says. So if a second wave hits and elective surgeries have to be curtailed again, “when do (hospitals) get a break? I am becoming skeptical — and I don’t have data to support it — I am becoming skeptical that even a year from now that we’re going to see a return to historical levels of hospital and physician utilization.”
Then there’s the problem of more patients who can’t pay. An April 3 analysis by consulting firm Health Management Associates reported that in an unemployment scenario in the midrange of projections — 17.5 percent — the number of California’s uninsured would grow by almost 200,000. Nationally, hospitals’ bad debt and charity care in March 2020 increased 13 percent over March 2019 and are expected to rise further, according to an April Kaufman Hall report.
The Long-Term Outlook
Even if small independent hospitals don’t close, they have tough decisions that will likely mean cutting services. Wipfli’s Johnson says they’ll need to figure out which service lines to keep and which to cut because their margins are low or negative. Subspecialties like orthopedics or physical therapy might get axed, he says.
More hospitals with cratering revenues also means that area businesses may need to budget for higher insurance costs next year: Hospitals and other providers could pass along some of their losses to private insurers. In March, Covered California warned that a lack of federal help could mean 40-percent hikes in insurance rates in the individual and employer markets next year. In June, a UC Berkeley School of Public Health study showed that the pandemic had cost California insurers about $2.4 billion for testing and treatment, six times the annual cost to treat the seasonal flu. Only two companies filed requests for health insurance rate changes with the state’s Department of Insurance between April and June. On June 1, Health Net requested a 4.1-percent annual average rate increase for one of its plans, and on June 3, Aetna requested an 8.2-percent bump for one of its own.
Orlov says one likely outcome is more mergers and acquisitions in Northern California’s already-consolidated hospital market. He predicts struggling hospitals will hang on for a while longer before declaring bankruptcy or being taken over. Oligopoly power has already driven up the region’s health care prices. “It’s going to be a real challenge for policymakers,” he says. “Do I let this tweener hospital close, or do I let Sutter take it over with its monopoly power? And it’s not going to be, from my perspective, an easy choice.”
“It’s going to be a real challenge for policymakers. Do I let this tweener hospital close, or do I let Sutter take it over with its monopoly power? And it’s not going to be, from my perspective, an easy choice.”
BERT ORLOV DIRECTOR, EISNERAMPER
There’s one glimmer of bright side for businesses that offer to cover their employees’ health insurance. Telemedicine — medical services by phone or internet — is here to stay, and studies show it can save a bundle on health care costs: $242 per episode of care, according to one study. Pre-coronavirus, most large employers offered telemedicine in their packages, but few employees actually used it. Now people have gotten used to talking to doctors remotely to stay out of waiting rooms. For smaller businesses, a telemedicine plan could be a more attractive perk now. Andrea Murphrey, a benefits consultant at Sacramento’s Capitol Health Management, says she offers a stand-alone telemedicine product that runs $10 a month and lets covered members contact a physician and get a prescription, which is the outcome in 70 percent of regular appointments, she says.
For now, hospitals are just trying to make it through the fall. “If we have seen the worst of it, or we’re very near seeing the worst of it, and Dameron can continue to execute on the strategy that we had in a pre-COVID world, I’m very optimistic about the combination between Dameron Hospital and Adventist Health’s ability to serve the community,” says Wolcott. “But it’s all an unknown due to COVID.”
–
Stay up to date on the effects of the coronavirus on people and business in the Capital Region: Subscribe to the Comstock’s newsletter today.
Recommended For You

Consumer Demand Will Drive Changes in the Health Care Industry
In our series, The Big Fix, industry experts explore how the region can rebound from the coronavirus shutdown
Just as businesses are adapting to support a remote workforce, significant changes are happening in how health care is delivered.

Status Check: Health Care Hanging On
Local leaders say they’re undaunted by intense fiscal impacts from COVID-19
COVID-19 has presented significant challenges for health care. At least for the moment, though, local providers have been hanging tough and looking toward economic recovery.

Health Care Jobs Spur Economic Optimism
Local economist says Capital Region’s strengths in health care sector help insulate it from effects of COVID-19
Health care and life sciences account for around 150,000 jobs in the Sacramento region, making the sector the largest private employer. Experts suggest that the public sector and health care may expand locally, even as the coronavirus pandemic contracts the global economy.

The Might of Medicine
With around 150,000 jobs, a robust provider marketplace and a slew of projects underway, health care helps define the greater Sacramento region
Though service gaps and challenges remain, health care could eventually become the Sacramento region’s calling card.