Like birth, the twilight season of life can be a painful passage. But for those who have the luxury of quality time with their elderly loved one, it can also be beautiful.
“You love them so much, you want them to have a special end chapter,” says Ann Evans, 73, who took care of her mother, Audrey, for the majority of the final months of her life before she died peacefully last year at the age of 100. “When they’re in your home, it’s just like having a kid. … They say things here and there, and you get all of that. … There are many moments of such tender joy, I wouldn’t give that up for anything.”
Evans, a retired food systems organizer and former mayor of Davis, wanted her mother to stay with her “until the end,” as is customary in her family. In many ways, she had the best of both worlds: Her mother’s income was low enough to qualify for Medi-Cal, which provided In-Home Supportive Services, while Evans and her husband were able to afford some supplemental care. But when Audrey could no longer walk and Evans’ husband was diagnosed with Parkinson’s disease, it became too much.
“I was more tired than I even knew,” says Evans. “Your life completely changes, and you kind of lose track of time, and you start being almost overwhelmed. ‘Is this ever going to end?’ But then you feel guilty because you think, ‘Oh, end means death,’ and I don’t want to be wishing for my parent’s death. But that’s the only way out.”
Evans’ mother lived with her for 13 months before moving into a $8,000-a-month board and care home. Typically licensed in California for six residents or fewer, board and care homes are “the best thing going,” according to Evans, though they can be competitive to get into. Audrey spent her final few months in the care of a husband and wife team, with frequent visits from her family. “It couldn’t have been nicer, but it wasn’t home, I knew that,” Evans says.
Now, more than a year after her mother’s death, Evans cries when describing a friend who is caring for an ailing husband. “I will help you because I know,” she says. “She’s not going to ask anybody for help, but I know you need it.”
It’s a hardship that so often falls on women but is rarely talked about. “It’s not a fun topic,” Evans explains, “and then you’re in it. … You’re losing yourself.”
A full-time job
Laurie Watkins had a feeling her dad wasn’t sharing everything about her mom. Her mother, Nancy, had suffered a suspected stroke a few years ago, and there were harbingers of advanced aging — shuffling feet, panic attacks, forgetting a birthday — that were concerning for a retired banking executive and doting grandma in her mid-70s. But it wasn’t until Watkins’ father was admitted to a lengthy hospital stay after quadruple bypass heart surgery and she moved in to stay with Nancy that she realized the true extent of her mother’s condition.
“She was a grown infant by this stage,” Watkins says. Her father had downplayed her mom’s diagnoses — Parkinson’s disease and Lewy body dementia — in an attempt to shield his children from worry, and he didn’t want to institutionalize his wife. But it was clear to Watkins that the care her mother had been receiving wasn’t enough. It was “a full-time job,” one that, at just 42 and with a child of her own, she had never planned for. Her mom needed help bathing, going to the restroom and getting out of bed. For eight weeks in the summer of 2023, Watkins took leave from work to be her mother’s live-in caregiver. She had joined what is often referred to as the sandwich generation — those who are caring for both their children and their aging parents. Concurrently, she was dealing with her own treatment for lymphoma.
“It was lonely. I couldn’t have a conversation with her anymore,” Watkins says of her mother, who was experiencing hallucinations, paranoia and bouts of uncharacteristic rage. Watkins missed her fiance and her teenage son, Mason, who was home alone for much of the day. “It was hard for me being away from him, knowing that time is fleeting,” she says. “I did a lot of thinking, just myself, at night time when it was quiet, and I would just think, ‘My god, how did time go so fast?’”
Nancy’s decline was very fast. By the end of the summer, she could no longer use her legs. Not expecting her to survive longer than six months, Watkins managed to secure hospice care, but the burden of her mother’s failing body was still too much to bear. One morning, Nancy fell while trying to get out of bed, and Watkins couldn’t lift her up. An ambulance came and took Nancy to the hospital, where she stayed for two manic nights before being admitted into a for-profit memory care facility in Citrus Heights, where she still lives today. Her cognitive health continues to deteriorate. “My mom’s gone,” Watkins says. “That is just a shell of who my mom used to be.”
Nancy’s board and care costs $7,000 monthly, according to Watkins — it was $5,500 when she moved in last summer — and she had to transfer into a shared room, as a private one now costs $14,000. Watkins says the price hike coincided with a change of ownership at the facility, which, for the memory care patients, is like a “locked-down prison” with ever-changing staff.
Going home isn’t an option for Nancy. Watkins needed to go back to work, and the cost of in-home care is unaffordable for the family at a median rate of $35 per hour in California, according to data collected by A Place for Mom. Nancy doesn’t qualify for Medi-Cal, either, due to her combined income with her husband, who is now living back at their home.
For middle-class families in particular, finding an ideal situation for Mom or Dad can be a labyrinth of closed doors and catch-22s. In January of this year, the asset limit for Medi-Cal was eliminated — a big win for advocacy groups and those who would have to sell assets and spend down to qualify for assistance — but the income requirement remains at 138 percent of the poverty level, which is $20,783 annually for an individual and $28,208 for a couple.
“Yes, there is a gap,” Debra Bonner, chair of Sacramento County’s Adult and Aging Commission, says about the plight of being in the middle. “Sometimes, if you talk to different agencies, you can work something out.”
No time to wait
There are plenty of resources for care in the Capital Region, but most people don’t seek them out until they’re already in a crisis.
“Don’t wait until something happens to figure this out,” says Heidi Richardson, program planner for the Senior and Adult Services Division of the Department of Child, Family and Adult Services in Sacramento County. “Start researching your options sooner rather than later so you’re not facing an emergency and trying to figure it out all at the same time.”
Richardson recommends starting with a call to the Aging and Disability Resource Connection, which helps people determine what kind of care they want and which services they are eligible for.
One of the best resources available for those with a prognosis of six months or fewer is hospice, which offers palliative care, emotional and spiritual support for the patient and their family wherever they call home. The cost is usually covered by Medicaid, Medicare and private insurance. Yet it’s common for patients or their loved ones to resist hospice care, not wanting to “give up,” according to Sheila Clark, president and CEO of the California Hospice and Palliative Care Association.
“We are not comfortable with facing death,” Clark says. “I know that it’s hard, but we want to give that gift of a peaceful death, and death’s not a dirty word. It’s not. We have to get comfortable with it.”
A collective trepidation extends to aging and caregiving, topics no one wants to think about until they’ve had a bad fall while home alone or when Grandpa can no longer drive. According to Clark, most people don’t realize what caregiving requires on a day-to-day basis. “Until you’re faced with it, you have no idea,” she says. “But we have to be able to give people grace. … We understand (if) you can’t be the caregiver.”
Again, Clark emphasizes the importance of advance care planning and planning well ahead with loved ones. For most Americans, the plan is to age in place — a 2021 AARP survey found that 77 percent of those over 50 want to remain in their homes for the long term. But that can require a lot of preparation, plenty of money and plain luck. For those who qualify for Medi-Cal, In-Home Supportive Services can help cover the cost of a caregiver, often a relative, but this requires a home that is accessible and safe.
“I think aging in place is kind of a privilege,” says Richardson. “There are people who don’t have homes to age into. We serve elders who are homeless, we serve elders who live in a room that they’re renting in a house, and that’s not their ideal preference. They don’t want to age in place in those situations.”
If all goes well
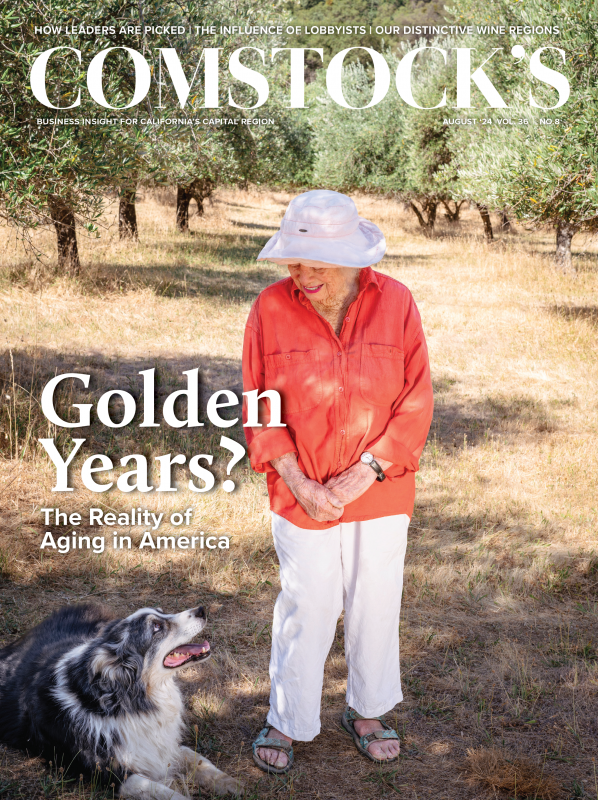
Susan Bragstad lives alone in a foothills farmhouse on the edge of town. It’s just her and her dog, Charlie — she’s divorced and has no children. “Never wanted any,” she explains simply. At 89 years old, she can deftly remark on the latest goings-on in politics and help out with the harvest of her 400-tree olive orchard. She is a woman of many lives: a San Francisco architect for several decades, an active environmentalist and the owner of Amador County’s eponymous olive oil company. She’s also the three-time former mayor of Amador City, and she’s not slowing down yet. “I’m just busy,” she says.
Susan Bragstad, 89, lives alone in the foothills with her dog,
Charlie. She plans to age in place and host a caregiver in an ADU
if she ever needs one. (Photo by Gabriel Teague)

When asked the secret to her vitality, she rattles off the trinity of wellness: good diet, regular exercise and socialization. But she mostly credits her genes. “Half my family is Syrian,” she says. “I think that helps with health.” She has a sister who is 92 and a family history of centenarians.
Bragstad has also been fortunate financially: “I bought Apple stock when it was $12 and Tesla when it was $16. I’m set.” Wearing a rather iconic pink wide-brimmed hat she’s been photographed in for various news articles, her gaze drifts fondly over the trees she planted, like old friends, having matured under countless summer suns. “How lucky can you be?” she asks no one in particular.
Even with the luck, getting old doesn’t come easy. “I feel it,” she says. “I had to have a friend help me yesterday to put some irrigation together, just because my muscles are disappearing. So I notice that, and I don’t like it.” And her friends keep dying. “It’s awful,” she laments. “But you have to get used to it if you’re going to live a long time.”
She’s also watched friends deteriorate and have to rely on the care of a relative. “They say it’s harder on the caretaker than the person. I don’t think my friend knew what was happening,” she says.
As for her own plans, Bragstad has “thought about it some,” and she has a spare unit that can host a caregiver. Still, her talk of the future is as nebulous as that of the distant past. About a year ago, she broke her ankle and had to call a friend to come help her. She’s fine now. “It’s in the background,” she says. “I don’t dwell on it because most of my friends are in the same boat.”
A correction was made on Aug. 19, 2024: It was inaccurately stated that Ann Evans’ mother’s board and care cost $4,000 monthly. It actually cost $8,000 monthly, according to Evans.
Recommended For You

Sleepy Suburbs? No Way
These Capital Region cities are buzzing with energy and ambition
A generation ago, Sacramento was the undisputed king of commerce and culture in our region. But the once-quiet suburbs are growing up fast. In fact, thanks to years of quiet community building, the edge cities are leading the way in defining the modern Capital Region.

The Changemakers
The people who’ve shaped the Capital Region over the past decade
The Capital Region has seen a stunning metamorphosis over the past decade. These changes didn’t happen on their own; they occurred due to the work and vision of a range of notable people, from developers and public officials to sports executives and innovators.

The Great Migration
From immigrants fleeing their countries to Bay Area residents escaping high prices, the culture of the Capital Region is changing
Just under 2.4 million people live in the Sacramento-Roseville-Folsom metropolitan area, an increase of roughly a quarter since the turn of the century.

Building the Future
Veteran architects are essential in mentoring young, emerging designers
The field of architecture is changing, and technology is playing a central role, but it’s not the only element that’s shifting: so is the expectation of what young and emerging professionals are looking for in an architectural job.

A Day in the Life of Comstock’s Publisher
Winnie Comstock-Carlson describes an average weekday as this magazine’s founder, president and publisher (for 35 years).

The Way We Work: Caroline Beteta
A glimpse into the daily life of the CEO of Visit California
On paper it’s a dream job of nonstop travel, but the reality is that most days she’s stuck in her office until 7 p.m. Thankfully she has a secret weapon: white space.