Doctors in the Capital Region aren’t just checking your temperature and blood pressure when you come in for a checkup these days; in growing numbers, they’re also checking your mood.
The major health systems in the region have taken steps to encourage primary care doctors to screen patients for behavioral health problems such as depression or anxiety. Some doctors routinely give new patients a brief questionnaire that can flag depression or include the screening tool as part of an annual physical exam.
Others are adding behavioral health specialists at primary care clinics to better coordinate care, or even hiring case managers to ensure that a patient diagnosed with depression is following through with treatment.
The goal here is the same as in similar efforts around the nation: Provide the best care for often-overlooked mental health problems, and catch them early — before they get worse and before the costs climb for treatment and lost productivity.
“It’s ethical care, it’s definitely best-practice care and it’s doing the right thing at the right time for the right patient,” says Dr. Richard Bowdle, director of medical affairs for the Sutter Center for Psychiatry in Sacramento.
Bowdle also serves as behavioral director for primary care in Sutter Health’s greater Sacramento region, making sure that the network’s doctors have the materials, screening tools and up-to-date education they need to treat patients who exhibit depression or other behavioral issues. Similar resources and education efforts are deployed at the other major health systems.
This is a national trend that’s gaining momentum, says Dr. Jaesu Han, assistant clinical professor in psychiatry at UC Davis Medical Center, who works with the primary care clinic on the university’s health campus in Sacramento. “We have a policy in the family medicine clinic that if you are a new â?¨patient, you get the screening,” he says, and so does any patient who requests it.
The trend has grown as more people recognize the scope and cost of the problem. More than 45 million people — almost 20 percent of all adults in the United States — experienced some form of mental illness over the previous year, according to a 2009 survey by the U.S. Substance Abuse and Mental Health Services Administration. Some 11 million, nearly 5 percent, suffered a serious mental illness; 1 million attempted suicide. Fewer than 4 in 10 received mental health services, the survey found.
“Too many Americans are not getting the help they need, and opportunities to prevent and intervene early are being missed,” said SAMHSA administrator Pamela S. Hyde in a news release when the survey results were announced in November. “The consequences for individuals, families and communities can be devastating.”
Primary care screening provides an early chance to identify
patients who need help, even if they don’t know why they feel
bad, says Dr. Robert Ruxin, chief of outpatient psychiatry in
south Sacramento for Kaiser Permanente. “A lot of people can’t
self-identify that they’re depressed,” Ruxin says.
“Depression is one of the major reasons for people calling in
sick to work, but they may present with physical symptoms” and
screening can help identify the underlying cause.
“Major mental disorders are very common,” Bowdle says. Research suggests 20 to 25 percent of adults may have one at some point in their lives. “If you don’t intervene early, the condition is likely to worsen … and the cost will spiral (up), both the cost of care and the loss of productivity.”
Primary care doctors — who through familiarity or insurance company rules are often the doctor a patient sees first — provide an opportunity for that early intervention.
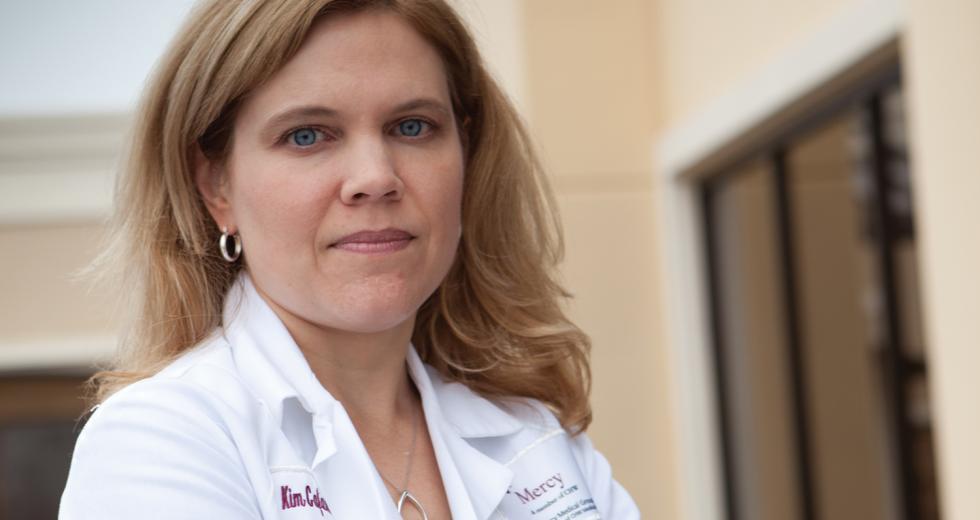
Dr. Kimberly Cafarella uses an in-house screening tool — and, if needed, has patients complete the 21-question Beck Depression Inventory survey — during all initial patient visits and at annual physical exams at the Mercy Medical Group’s Folsom clinic. The clinic has a therapist on site, and integrating primary care and behavioral health is a common topic for continuing medical education courses within Mercy, she says. “The two are so intertwined that you really have to look at both.”
Sutter has been promoting the use of another screening self-test, known as the PHQ-9, which is both sensitive and specific, Bowdle says; nearly 80 percent of those who score high on the depression test have the diagnosis confirmed by a doctor. Starting in January, Sutter launched a pilot project to conduct follow-up PHQ-9 tests every three months for a year to track progress and which treatments work best.
Kaiser also uses the PHQ-9, and has launched a pilot to track patient symptoms online, says Dr. Steve Melcher, chief of inpatient psychiatry for Kaiser’s Sacramento region.
Kaiser, a combined health system and insurer, was early to recognize both the medical and financial benefits of integrated care and began adding behavioral specialists at primary care clinics years ago. About a year ago, Ruxin says, Kaiser added a psychiatrist at a clinic in San Francisco, and in December it added one in south Sacramento.
Other insurers see the advantages, too. Aetna, for example, is paying some 5,000 primary care doctors to administer the PHQ-9 and is training behavioral health specialists for primary care clinics. The federal health care reform bill also encourages better integration of physical and behavioral care by 2014.
Initial screening doesn’t do much, though, if there’s no follow-through on treatment, and there’s still a stigma in the minds of many patients about seeking help for mental health problems. That’s why the family clinic at UC Davis Medical Center is adding a case manager, who this month will begin contacting patients to make sure they take their medicine and show for follow-up appointments.
Recommended For You

Rational Approach
Managing mental health in the workplace
A few years ago, Troy Underwood noticed a problem with one of his accountants. The man’s work performance and personal appearance had deteriorated, he talked constantly on the phone with his children and agonized about his domestic life.
Diagnosis Dilemma
Mental illness is often overlooked in aging populations
Until about a year ago, 86-year-old Clair was living in her own home on the East Coast with her husband of 60 years. When her husband died suddenly, her daughter quickly moved Clair into a senior living complex in Sacramento to be near family.